|
In 2010, coronary artery disease remains the number-one killer in all age groups in the United States. The statistics for women are particularly sobering - nearly 1 in 3 women die from coronary artery disease (CAD) compared to nearly 1 in 5 from Cancer.(1) African-American women are 35% more likely to die of heart disease than Caucasian women, while Hispanic women face heart disease nearly 10 years earlier than Caucasian women. Pacific Islander women, long considered at low risk, count heart disease as their second leading cause of death. Obesity, high cholesterol, poverty, language barriers, physical inactivity, and lack of information all contribute to increased risk and a recent study found that minority patients might have poorer health because of disparities in health care delivery, while another found that minority women were more likely to mistrust their health care provider.(2)
Misconceptions about heart disease as it affects women
Misconceptions about women's heart disease grew roots decades ago. In the 1960s, erroneous assertions that heart disease was primarily a man's disease were widely spread to the medical community and to the public. This led to research almost exclusively focused on cardiovascular disease in men. Many clinical trials in the 70's and 80's excluded women or simply didn't make an effort to enroll women in sufficient numbers to draw gender-based conclusions. The lack of relevant research in women has resulted in a substantial gender-based knowledge deficit about everything from the "typical" heart attack symptoms in women, to the risks and benefits of commonly used diagnostic tests and therapies. In current cardiovascular research, we are not necessarily analyzing the data by gender and the need for gender-specific studies is not on the radar screen of researchers. In addition, it is more difficult to recruit women for these trials. Too many women do not think of heart disease as a "woman's" disease, so they don't see the relevance or potential benefit of seeking out and participating in clinical trials. Therefore, the published guidelines are less likely to be applied to women compared to men. Additionally, many women in the U.S. receive all or most of their medical care from their obstetricians or gynecologists. Traditionally, there has been a greater focus on reproductive and breast health in women than on their other health risks, and conversely, a lower awareness among obstetricians and gynecologists about identifying and treating signs of heart disease.
Cost versus accuracy of test results
Other fundamental issues remain, such as the prohibitively high cost of the available diagnostic stress-imaging tests, which are beyond the reach of most poor, uninsured, and minority populations. These tests often impose other long-term risks on patients, such as unacceptable exposure to cancer causing radioactive isotopes, ionizing radiation, and intravenous contrast materials. Those who can afford and have access to these tests risk potential over-exposures when tested repeatedly. These stress-imaging tests often fail to detect women with single vessel or multiple vessel disease (3), with or without critical stenosis(a). Noninvasive diagnostic testing for detection of CAD in women presents challenges not encountered in men. Prevalence of CAD in women, even with typical angina, is lower compared to men, thus reducing predictive accuracy due to commonly applied Bayesian principles. Female patients also more frequently have single-vessel disease and intermediate grade stenosis (defined as having 1-49% coronary artery blockages)that in combination with smaller heart sizes imposes additional difficulties for stress tests to identify abnormalities. A recent evidence-based report from the U.S. Agency for Health Care Research and Quality stated that the accuracy of exercise ECG and thallium single-photon emission computed tomography (SPECT) for the diagnosis of CAD is lower in women than in men due to both poorer sensitivity and specificity. While the accuracy of exercise echocardiography is believed to be better than either stress-ECG or -SPECT, this assertion is supported by limited data from studies that included only 296 women.(4) A separate issue is that assessment of the quality of stress testing trials is difficult as these data are frequently subject to different forms of bias-mainly pre-test, work-up, or post-test referral bias-which hampers calculation of test accuracy.(5) Finally, exercise echocardiography is technically demanding and not readily accessible to those who cannot afford it, particularly the uninsured or those who have no access to specialty medical care.
The biology of women's heart disease still remains unclear. Women have more angina or chest-pain with less obstructive CAD, and more myocardial ischemia compared to men. Normal epicardial coronary arteries are seen more frequently in women with chest-pain than men. Women also have worse clinical outcomes compared to men. In addition to microvascular reactivity and endothelial dysfunction with abnormal coronary perfusion, vascular problems, autoimmune problems, migraine headaches and Raynaud's phenomenon or vaso-spastic disorders, or the phenomenon of the so-called "Broken Heart Syndrome" affect more women than men. Women have a higher mortality compared to men with acute myocardial infarction. In the recent NIH sponsored Women's Ischemia Syndrome Evaluation or the "WISE" study,(6) the 5-year annualized cardiovascular event rate was 16% in the "WISE" women with suspected ischemia due to non-obstructive CAD(a), 7.9% in "WISE" women with suspected ischemia, but having "normal" coronary arteries, and 2.4% in asymptomatic controls. However, the good news is that if diagnosed early, medical treatments using Statin drugs, ACE inhibitors, and Beta-Blockers, combined with life-style change, proper nutrition, and exercise, women with coronary artery disease may enjoy a long-term prognosis similar to men.
The central issue in this discussion is that there is an urgent need for a more accurate, safer, cheaper, and readily accessible non-invasive diagnostic tool to detect coronary heart disease in a timely manner so that effective medical treatments can be delivered early and adverse events are prevented.
Recently, a little known and potentially "disruptive" 21st-Century high-tech solution has become available - the Internet based MultiFunction Cardiogram or MCG. The MCG is an affordable, non-invasive, Internet-based, systems-analysis tool without IV contrast, stress and radiation that addresses a fundamental tenet of medicine - "First, Do No Harm". The technology utilizes the MCG field data collection unit as an "Internet Appliance", a small electronic portable device, to collect the patient's resting surface ECG data from leads II and V5, and generate a mathematical model designed for the detection of all stages of chronic and/or acute, local and/or global myocardial ischemia due to underlying coronary artery disease. The MCG can detect ischemia caused by as little as 30-40% single vessel coronary obstruction (7) up to very severe multiple vessel coronary obstruction with similar or better accuracies than the current more expensive stress-imaging modalities. It is able to accomplish this by eschewing traditional time-domain ECG waveform analysis in favor of an entirely new methodology based on a multifunction mathematical analysis of the electro-mechanical function of the heart in the frequency and time domains, and an analysis of the integrity of that function over multiple cardiac cycles, not a small portion of one cycle. It is the first of its kind adapting the mathematic principal of LaGrange-EŁler Coordinates (8) to build a mathematic model of the human heart using it to measure the interaction between myocardium and intra-cardiac blood flow.
How the MCG works
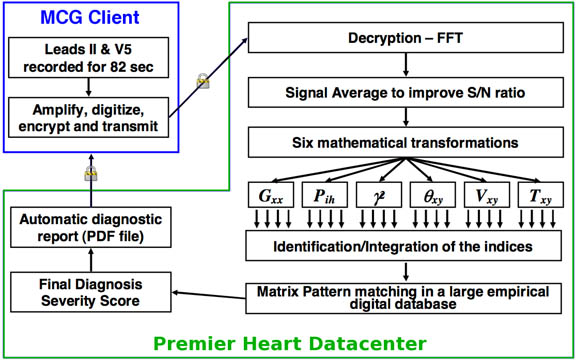
Operationally, the MCG technology uses an easy to operate portable device at the point-of-care site to harmlessly record multiple cycles of resting ECG analog signals from leads II and V5 of a patient, then digitizes, encrypts and securely transmits the resting ECG data along with the patient's demographic information to a central data center for processing. After receipt of the data by the server, the system performs a Fast-Fourier-Transformation of the signals from each lead, preparing them for further mathematical transformations which have been discussed elsewhere.(7&8) These mathematical transformation functions comprise the backbone of the systems-analysis "engine" which evaluates the dynamic interactions between heart muscle chambers and the intracardiac blood flow. Abnormal expressions of these functions can assist physicians in the detection of coronary ischemia from very early to very late stages. The functions are used to extract the non-linear functional relationships between the two leads, which are distilled to a set of indices, and then matched against existing patterns in a large 40,000 patient empirical database to determine the presence or absence of local and/or global ischemia, and produce an overall disease severity score, 0 to 20, completely unlike the conventional ECG technologies currently known to physicians. The entire process takes literally a few minutes. (See Figure below for an overview of the MCG process).
The MCG obtains information from the electromechanical data imbedded in the two resting ECG leads, which no one realized was available to evaluate until now. Instead of merely retrieving summed information about the electrical activity of cardio-myocytes at a single time point during a single cardiac cycle by convention, MCG obtains information about the dynamic interface of the myocardium and intracardiac blood flow over multiple complete cardiac cycles. This makes it possible to model, quantify, and understand the ongoing stress-strain interaction between the myocardium and intracardiac blood flow resulting in the ability to directly identify chronic or acute ischemic alterations that are less intense than the traditional ECG can measure. The traditional ECG techniques, using only diagnostic surrogates, typically only indirectly identify acute, more intense ischemia affecting a larger portion of the heart (i.e., many more myocytes simultaneously). Another way to think about the relationship of MCG to the conventional EKG is to relate it to that of high-speed Internet access and dial up access - both of which can be transmitted over the same telephone lines, which no one realized was possible until a few years ago. More than two decades have past, the workers of MCG technology pioneering the "roads-less-traveled",(9) have built a first-of-its-kind reference digital clinico-pathological database which contains validated MCG and coronary angiographic data from more than forty thousand individuals ranging in age from 14 to 99, with equal numbers of women and men. More than twelve thousand patients in the database represent normal individuals over the same age range, with equal numbers of men and women. This design of the database is used to normalize the mathematical calculations and minimize age and gender-based bias. The use of this type of large, well-designed, database that includes 20,000 women of all ages as a comparator in the analysis of each patient's MCG data is unprecedented and is in direct contrast to the studies in the medical literature focusing only on middle-aged men conducted in the 70's, 80's and 90's. To further highlight this issue, the studies of exercise echocardiography in the literature, mentioned and cited above, included less than 600 women.
MCG reliability and safety
Over the years, this Internet-based high-tech method and its uniquely normalized reference-digital-clinico-pathology database have been retrospectively verified and prospectively validated to be very accurate over tens of thousands of people. The goal of this new technology is to build a physician-directed, office-based, cost-effective, non-invasive point-of-care system, which is a highly accurate detector (of CAD and other forms of heart disease) potentially reducing or bypassing the need for stress-imaging, coronary computed tomography, or diagnostic coronary angiography. To prove these claims, MCG data has been compared directly to coronary angiography in several carefully designed and well-conducted prospective double-blind clinical trials (10, 11, 12, & 13) in which it detected CAD ischemia with over 87% accuracy. This is the highest diagnostic accuracy reported in the medical literature when compared to other stress-imaging tests currently in use. The MCG clinical trials asked a different question than that normally being asked, namely, whether MCG could accurately detect which patients, from a group whose physicians believed needed coronary angiography, actually did need coronary angiography because they had relevant (>70%) coronary stenosis. In other words, MCG claims to do more than just "evaluate" patients who are at low or intermediate risk of having coronary artery disease, as a first step in the traditional diagnostic chain: It's capabilities render other diagnostic tests unnecessary and potentially allow selected patients to proceed directly to coronary angiography for timely intervention or to start medical treatments for those who did not require angiography. MCG also allows physicians to monitor the progress of their patients conveniently at much lower costs. This direct comparison of a two-lead-resting ECG system with the gold-standard coronary angiography is unheard of in the medical literature from 1949 to now, and represents a paradigm shift in CAD detection offering opportunity in early detection/prevention, disease monitoring and timely intervention, if indicated.
Cost-saving breakthrough technology
Many physicians in the US and Internationally, following a full review of the underlying biomathematics and basic science of the MCG technology, a review of the prospective MCG clinical trials design and data analysis, and their first-hand clinical experience with the device in their clinical practices, have found that the MCG is a well-validated diagnostic tool, and, that if used early in a symptomatic patient's evaluation, is able to very accurately predict which patients, equally accurately for men or women, who are considered "at low or intermediate risk" of coronary artery disease by ACC/AHA 2002 criteria(14), actually do not have relevant coronary stenosis
(defined as coronary artery blockages of >70% in one or more major epicardial coronary vessels or >50% left main stenosis which may require percutaneous or surgical coronary intervention)
at the time of examination. According to the evidence generated from and the statistical calculations based on the existing clinical trial data, MCG has demonstrated a very high ability to rule out hemodynamically relevant coronary stenosis (>70%) in subjects with very low to intermediate risks (With Negative Predictive Value or NPV > 90% for risk < 50%; NPV > 97% for risk < 20%). Therefore, MCG is, from a statistical perspective, well suited to prevent unnecessary coronary angiography in patients with low to intermediate "a priori" risk of CAD (defined by a knowledge of the actual population rates)(15).
One practical consequence of this is that when MCG is employed early in the patient's evaluation, a significant number of patients will not likely need to undergo any form of "add-on" stress-imaging testing, angiography, or even hospital admission if their MCG severity scores are low (For example, the patientís MCG disease severity score is below 4.0) Because MCG testing can be performed at the point of care, the management of these patients can be dramatically improved and the overall cost of care reduced. No other ECG-based diagnostic technology has been able to make this type of determination with the accuracy of the MCG has demonstrated. In the typical community setting, most patients experiencing symptoms of chest pain will be seen first by their internist, family physician, or in case of a woman, her Obstetrician/Gynecologist. With proper support and implementation, if MCG testing is performed by the primary care physicians and confirms a very low likelihood of relevant coronary stenosis, evaluation and treatment can potentially continue without the need for cardiology consultation and/or additional "add-on" telescoping of time consuming and costly ECG stress, or stress imaging tests. The MCG score could also easily be incorporated as a pre-certification screen for any subsequent "add-on" testing by Medicare or Commercial carriers.
Conclusion
These current turbulent economic times dictate an imperative to provide the best possible quality care at an affordable cost to all, especially those who are under-represented and under-served. The MCG is a cost-effective Internet based high-tech diagnostic tool. It is our belief that if the MCG is systematically adopted and used as a gate-keeping mechanism in the hands of primary care practitioners, family medicine groups, OB/GYN specialists, urgent/emergent care physicians, internists and cardiologists, it will result in substantial savings of U.S. healthcare dollars, improve access to care for women, minorities and the uninsured and improve outcomes for all. In managing our #1 disease burden - heart disease - MCG is the best tool that modern medicine can offer.
About the Authors:
(I) Marina Vernalis DO, FACC, Former Chief of Cardiology, Walter Reed Army Medical Center
(II) John E. Strobeck, MD, PhD, Founder and Medical Director of Heart-Lung Associates of America, PC, and a Consulting Editor of Congestive Heart Failure Journal.
(III) Charles Miceli, MD, cardiologist and internist who has personally tested more than 2,000 patients using MCG technology and is now an expert in MCG clinical applications.
(IV) Joseph T. Shen, MD, Co-inventor and MCG Technology developer, Founder of Premier Heart, LLC. www.premierheart.com For reprints, questions or comments, please email Dr. Shen at jtshen@premierheart.com
Citations:
1 . Shaw et al. JACC vol. 54. no. 17, 2009
2. Anita B. Varkey; Linda Baier Manwell; Eric S. Williams; Said A. Ibrahim; Roger L. Brown; James A. Bobula; Barbara A. Horner-Ibler; Mark D. Schwartz; Thomas R. Konrad; Jacqueline C. Wiltshire; Mark Linzer; for the MEMO Investigators. Separate and Unequal: Clinics Where Minority and Nonminority Patients Receive Primary Care. Arch Intern Med., 2009; 169 (3): 243-250 [link]
3. Dr. Jennifer H. Mieres Heart Smart for Black Women and Latinas, and a Women Heart advisor
4. Diamond GA. Reverend Bayes' silent majority. An alternative factor affecting sensitivity and speci?city of exercise electrocardiography. Am J Cardiol 1986;57:1175- 80.
5. Cecil MP, Kosinski AS, Jones MT, et al. The importance of work-up (veri?cation) bias correction in assessing the accuracy of SPECT thallium-201 testing for the diagnosis of coronary artery disease. J Clin Epidemiol 1996; 49:735- 42.
6. Adverse Cardiovascular Outcomes in Women with Nonobstructive Coronary Artery Disease. Arch Intern Med/vol. 169 No. 9 May 11, 2009.
7. Weiss MB, Narasimhadevara SM, Feng GQ, Shen JT. Computer-enhanced frequency-domain and 12-lead electrocardiography accurately detect abnormalities consistent with obstructive and nonobstructive coronary artery diseases. Heart Dis. 2002;4:2-12.
8. Feng G. EKG and EEG Multiphase Information Analysis (A collection of unpublished notes, thesis, papers and published articles from mid seventies to the late eighties translated into English from Chinese), First Edition. USA: American Medical Publishers; 1992.
9. "Roads Not Traveled" by Robert Frost
10.. Weiss MB, Narasimhadevara SM, Feng GQ, Shen JT. Computer-enhanced frequency-domain and 12-lead electrocardiography accurately detect abnormalities consistent with obstructive and nonobstructive coronary artery disease. Heart Dis. 2002;4:2-12.
11. Grube E, Bootsveld A, Yuecel S, et al. Computerized two-lead resting ECG analysis for the detection of coronary artery stenosis. Int J Med Sci. 2007;7:249-263.
12. Grube E, Shen JT, Imhoff M, et al. Computerized two-lead resting ECG analysis for the detection of coronary artery stenosis after coronary artery revascularization. Int J Med Sci. 2008 5(2):50-61
13. Joji Hosokawa, MD, PhD; Joseph T. Shen, MD; Michael Imhoff, MD, PhD Computerized 2-Lead Resting ECG Analysis for the Detection of Relevant Coronary Artery Stenosis in Comparison With Angiographic Findings Congest Heart Fail. 2008;14:251-260.
14. Raymond J. G, Gary J. B, J. Timothy B, et al. ACC/AHA 2002 Guideline Update for Exercise Testing A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing).
15. Strobeck JE, Shen JT, Singh B, et al. Comparison of a two-lead, computerized, resting ECG signal analysis device, the MultiFunction-CardioGram or MCG (a.k.a. 3DMP), to quantitative coronary angiography for the detection of relevant coronary artery stenosis (>70%) - a meta-analysis of all published trials performed and analyzed in the US. Int. J. Med. Sci 2009;6(4):143-55.
Acknowledgments:
We would like to thank Bonnie Arkus of the Women's Heart Foundation for inviting us to publish this article and Michael Graziano for his excellent editorial input.
-- end --
|

























